FAQ
Here are some of our frequently asked questions. Click on the question to reveal the answer below. If you have any questions that are not covered below, please contact us on 01366 386666 and we will be happy to help.
We are always pleased to welcome new patients. Please call in to speak to one of our receptionists or telephone the practice on 01366 386666 in order to arrange an initial examination. What can I expect at my initial examination? First visits are very important for both dentist and patient. At an initial examination, we will discuss previous dental and medical history, any concerns you may have, as well as conducting a thorough examination of your oral health. The initial examination will include: How do I get to the practice and where can I park? The practice is located at 5 Priory Road, Downham Market. For sat-nav users our postcode is PE38 9JU. There is a free, long stay public car park directly opposite the practice (next to Discover Downham Heritage) with a pedestrian crossing close by. There are also parking bays just after the surgery, on the right-hand side of the road, where you can park for up to 1 hour. Downham Market Train Station is a five-minute walk away, as is the bus station, which is situated by the side of Morrisons. Our two closest bus stops are in Priory Road (near Tesco’s) and Trafalgar Road. Please telephone reception for directions if you are unsure and we will be happy to help. Good value is important in dentistry and we don’t want finance to be a barrier to your dental treatment. We will provide a written estimate of the anticipated cost of any planned treatment and ensure that you fully understand when payments are due. We operate a “pay-as-you-go” system which means that payment for your treatment will be due on each visit. Treatment involving a laboratory fee will need to be paid for in advance of completion. Where clinically possible, the dentist may be able to spread your treatments to suit your finances. Once dentally fit, there may be the option of joining Denplan Care, our comprehensive dental payment plan. What is Denplan Care and how do I join? Denplan Care is a dental payment plan where you pay a fixed monthly amount to cover the cost of your routine care. Having Denplan Care means you won’t receive any unexpected dental bills. Denplan Care covers all the routine care you need to keep your teeth and gums healthy, including examinations, x-rays, hygiene treatment, fillings, root canal treatments, crowns, bridges, dentures, onlays and inlays (laboratory fees, prescriptions, cosmetics and referrals are excluded). Needless to say, your teeth are an extremely essential part of your body. Apart from helping you to chew your food, your teeth contribute a lot towards your overall appearance. Therefore, it is very important for you to take care of them so that they last you a lifetime. X-rays help your dentist to find problems early on, so that they can be treated before they get worse. Early treatment generally costs a lot less as well. Although a tooth may look healthy on the outside, tooth decay can often be present in between teeth or under fillings, which is not always possible to detect on a visual inspection. X-rays can also be used to identify infections in the root, missing bone around the teeth, the condition of wisdom teeth and to detect the growth of adult teeth in children. Are X-rays harmful? There is a very small risk involved with any exposure to radiation but technological advances in the X-ray equipment used means that the radiation dose from a dental X-ray is extremely small and the actual risk is negligible. To help you understand the level of risk involved, we have compared the amount of radiation you will receive when having dental and medical X-rays, with 1 year of natural background radiation. X-ray Type = Additional background radiation Another comparison would be travelling by air. A flight to Spain and back from the UK, would expose you to the same radiation as having two dental bitewing X-rays. I’m pregnant – should I avoid having X-rays? Evidence shows that there is no perceptible risk to the baby or the mother, so we should be able to take routine dental X-rays, however we will discuss this with you before proceeding. The hygienist plays a very important part in your dental care. The hygienist is mainly concerned with gum health – professionally cleaning your teeth (known as a ‘scale and polish’) and showing you how to keep your teeth and gums free of plaque. Plaque is a soft, sticky film of bacteria that constantly forms on your teeth. If the plaque is not effectively removed by brushing and flossing, over time it will harden to become calculus (tartar) which can only be removed by a dentist or hygienist. If plaque and calculus are allowed to build-up, it can lead to gum disease. Left untreated, gum disease can progress until the teeth become loose, fall out or have to be extracted by a dentist. In fact, more teeth are lost through the latter stages of gum disease than through tooth decay. What is gum disease? Gum disease describes swelling, soreness or infection of the tissues supporting the teeth. It can occur at any age, but it is most common in adults. There are two main forms of gum disease; gingivitis and periodontitis. What are the signs of gum disease? Unfortunately gum disease tends to progress slowly and painlessly so you may not be aware of the damage being done. The first sign of gum disease is blood on the toothbrush or in the rinsing water when you clean your teeth. Your gums may also bleed when you are eating, leaving a bad taste in your mouth. Your breath may also become unpleasant. Why should I use floss or interdental brushes? Brushing twice a day is essential, however, even with the most thorough brushing technique, it is not possible to remove plaque and food particles from in between the teeth with a regular toothbrush. Regular interdental cleaning (cleaning between the teeth) is just as important as tooth brushing as it is a high risk area for both gum disease and tooth decay to develop. Sugar causes tooth decay but, the essential thing to remember is that, it is not the amount of sugar in the diet, but how often it is eaten or drunk which is important. How can I avoid tooth decay? Consuming sugary or acidic foods and drinks between meals will increase the risk of decay, as the teeth come under constant attack and do not have time to recover. Therefore the best way to avoid tooth decay is by eliminating sugar from your routine daily diet, having sugar-free snacks like carrots, celery or cheese, and limit sugar consumption to special occasions only. What happens to decayed teeth if I just leave them? If left untreated, matters can get worse and you may lose a tooth that could otherwise have been saved. In the early stages of tooth decay there may be no symptoms. However, left untreated, tooth decay will spread further into the tooth, reaching the nerves and blood vessels (the pulp), and can cause pain and sensitivity. Once decay reaches this stage, damage to the nerves and blood vessels can cause the tooth to die and you may develop an abscess. A dead (or dying) tooth will require root canal treatment in order to save it. If root canal treatment is not possible, the infected tooth will need to be extracted. Root canal treatment (or endodontics) is needed when the nerves and blood vessels of the tooth (the pulp) are infected through tooth decay or injury. When the pulp becomes infected, the nerve of the tooth will begin to die. The infection may spread down the root canal system of the tooth, into the bone at the tip of the root, and may eventually lead to an abscess. An abscess is an inflamed area in which pus collects and can cause pain and swelling of the tissues around the tooth. Why not just take antibiotics for a tooth infection? Antibiotics cannot cure a tooth infection, they can only offer temporary relief. Antibiotics can only work by reaching the site of the infection through your blood. When a tooth is infected, the blood vessels in the tooth are damaged so the antibiotics are not able to get inside. The antibiotic will go everywhere else in the body, so it will help fight the infection in the surrounding tissues, but it cannot enter the tooth. The only way to save the tooth is to carry out root canal treatment to remove the dead tissue causing the infection. Tooth erosion – also known as ‘dental erosion’ or ‘acid erosion’ – is the loss of tooth structure (enamel and dentine) which is dissolved away by acid in the diet. The main cause of erosion is from acidic foods and drinks, like fruit and fruit juices, particularly citric ones (like lemons, oranges and grapefruits), and fizzy drinks (like cola and lemonade). When these acids are consumed they soften the enamel. Your saliva will slowly neutralise the acid in your mouth, getting it back to its natural balance and allowing the enamel to re-harden. However, if these acid attacks happen too often, your mouth does not have a chance to repair itself and tiny particles of enamel will be dissolved away. Over time, the enamel becomes thinner, exposing the soft dentine underneath, which can lead to pain and sensitivity. Eroded teeth are also more likely to suffer tooth decay. What can I do to prevent tooth erosion? There are a number of things you can do to help prevent erosion: – It is also important to remember that tooth erosion will be made worse if the teeth are brushed within an hour or two of consuming acidic food or drinks. This is because the acid softens the tooth enamel and then the toothbrush acts as an abrasive, removing the softened surface layer of the tooth. If left undisturbed for at least an hour, the enamel will have the chance to harden and remineralise. Having sensitive teeth can mean anything from a mild twinge to severe discomfort that can last for several hours. It can also be an early warning sign of a more serious dental problem. You may find that hot, cold, sweet or acidic foods and drinks can bring on sensitivity, so you may want to avoid these. If you have sensitivity when brushing your teeth with cold water try using warm water instead. It is very important not to avoid brushing your teeth as this could make the problem worse. A crown (also known as a ‘cap’) is an artificial restoration that fits over a prepared tooth, making it stronger and giving it the shape of a natural tooth. They are usually made from porcelain, ceramic or gold alloy. After consultation with the dentist, you will be made two appointments. At the first appointment, the dentist will prepare the tooth to the ideal shape for the crown. Once the tooth is shaped, the dentist will take an impression (mould) of the prepared tooth, and also one of the opposite jaw to register the way you bite together. Where possible, the dentist will fit you with a temporary crown to cover and protect the prepared tooth, and the impressions will be given to a dental laboratory technician, who will make the final crown. At the second appointment the temporary crown will be removed. The dentist will sit the new crown over your tooth to see if it is the right colour, shape and fit. Once you are both happy with how it looks, the dentist will cement the crown firmly into place. Your appearance is one reason to replace missing teeth. Another is the effect missing teeth can have on your oral health. The space left by a missing tooth can put a greater strain on the teeth at either side. A gap can also mean your “bite” is affected, because the teeth next to the space can lean into the gap and alter the way the upper and lower teeth bite together. This can then lead to food getting trapped in the gap, which can cause both tooth decay and gum disease. Your appearance is one reason to replace missing teeth. Another is the effect missing teeth can have on your oral health. The space left by a missing tooth can put a greater strain on the teeth at either side. A gap can also mean your “bite” is affected, because the teeth next to the space can lean into the gap and alter the way the upper and lower teeth bite together. This can then lead to food getting trapped in the gap, which can cause both tooth decay and gum disease. Partial dentures Bridges Dental implants A partial denture is a removable plate with a number of artificial teeth on it. It may be all plastic or a mixture of metal and plastic. Dentures are held in place by their natural suction to your gums. They may also have clasps to help keep them in place in the mouth. Dentures are custom made to fit your mouth so you shouldn’t normally need a denture fixative, however, over time, dentures may become loose and not fit as well. When this happens, some people prefer to use a fixative for a short time before having them relined or replaced. Studies show a smile is hugely important to our personalities, self-confidence, relationships and success. If you’re feeling self-conscious about your teeth, or just want to improve your smile, there are various dental treatments that we can offer to help you achieve a more beautiful, confident smile. Stained or discoloured teeth Extrinsic discolouration can be caused by: Intrinsic discolouration can be caused by: Combination stains: Treatment – Depending on the severity of the discolouration or staining, there are different options available to correct this. It can often be as simple as a visit to the dental hygienist for a scale and polish or replacing old fillings with new tooth-coloured ones. Discolouration or staining that cannot be removed by professional cleaning or replacement fillings can usually be treated with tooth whitening and/or veneers, however your dentist will advise you on the treatment options available to you. Tooth whitening Over-the-counter tooth whitening kits are sold in most major pharmacies and online stores. These kits will only contain weak hydrogen peroxide, so may not be as effective as the stronger professional products used by your dentist. Some products that you can buy over the counter are more effective than others, depending on how much bleaching ingredient they contain. Some cheaper whitening kits work by simply dehydrating the teeth which causes a lightening effect, however once you stop using the product and the teeth are rehydrated (usually a few days), they will begin to return to their original colour. If you’re considering using an over-the-counter tooth whitening kit, make sure you select a product which carries the logo of the British Dental Health Foundation and consult your dentist before proceeding. Veneers Veneers maybe used when: Ideally, as soon as their first tooth makes an appearance, start taking them to the dentist. By taking your child to the dentist regularly – usually once every six months – we can catch any potential problems before they appear or become painful. We can also offer you advice and information on how to keep your child’s mouth healthy, as well as preventative treatments (where necessary), like fissure sealants. When will my child’s teeth come through? Normally the primary (baby) teeth start to appear in the mouth at around six months after birth. For each tooth type, the lower teeth tend to appear about two months before the upper teeth. By two to three years old most children have their full set of 20 primary teeth, that is five on each side of the midline of the top and bottom jaws. As your child grows the jaws grow and spaces may begin to appear between the primary teeth. This growth makes space for the permanent teeth, which are usually larger than the primary teeth. The growth in jaw length also accommodates the permanent molars, which will appear behind the primary teeth. The first permanent teeth to appear are normally the four 1st permanent molars. These erupt at around age six years behind the primary teeth. Why fill baby teeth when they will eventually fall out anyway? Decayed baby teeth can cause pain, abscesses and infections, and can affect the permanent teeth. Your child’s general health can also be affected by diseased teeth so it is very important to get treatment as early as possible. Should my child use fluoride toothpaste? Fluoride comes from a number of different sources, including your drinking water (depending on where you live). Fluoride is highly beneficial to dental health. It helps strengthen tooth enamel which makes it more resistant to tooth decay. Most toothpastes now contain fluoride so these should provide you and your family with enough fluoride to benefit your teeth. If you are more prone to tooth decay, your dentist may advise the use of a fluoride supplement. However, it is very important that fluoride supplements are only taken on the advice and instruction of a dentist, as excessive fluoride can cause ‘enamel fluorosis’ in children. In severe cases, ‘enamel fluorosis’ can cause the enamel to become pitted and discoloured, which may look unsightly. There are many different brands of children’s toothpastes on the market – always use a children’s toothpaste suitable for their age group – this will be clearly indicated on the packaging. If you are unsure about using fluoride toothpaste, ask your dentist, health visitor or Health Authority. What are fissure sealants? The top surfaces of your teeth (the chewing surfaces) aren’t smooth and flat. They are criss-crossed with tiny hills and valleys called pits and fissures. These are places where plaque can build up safe from your toothbrush and dental floss. Some of the pits and fissures are so narrow that even a single bristle from a toothbrush can’t get deep enough to clean them out. We include oral cancer screening at every routine examination, so it’s important to visit your dentist regularly. The earlier oral cancer is diagnosed, the better your chances of recovery. You can download and save the ‘Do-it-yourself’ mouth cancer check by clicking here – Download Mouth Cancer Check PDF Other symptoms can include: These symptoms aren’t always caused by oral cancer but if you have any of them, or are concerned about anything unusual in your mouth, please contact your GP or dentist without delay and make sure they know your worries. What causes oral cancers? Excessive alcohol consumption, smoking, chewing tobacco, poor diet and HPV (human papilloma virus) are all significant risk factors for developing oral cancer – those who both smoke and drink to excess are up to 30 times more likely to develop the disease. Prevention is key and lifestyle choices can reduce significant threats of mouth cancer. For more information on mouth cancer please visit: www.mouthcancer.org Dental emergencies can occur at any time and whether it is a broken tooth or dental abscess that is causing you pain, prompt treatment and advice can make all the difference to sorting out the problem. Dental emergencies can be extremely stressful and cause a lot of pain. If you have a dental problem, please call us as soon as you can. We aim to see, or give advice to, all registered patients with genuine dental emergencies on the same day they contact us – please call us as early as possible to ensure your best chances of getting help the same day. Out of Hours If you are a Denplan patient, and you have the ‘Supplementary Insurance Cover’ included in your Denplan policy, you will be covered for dental injuries and severe dental emergencies both in the UK and abroad. You can contact Denplan’s 24-Hour Worldwide Dental Emergency Helpline on 0800 844 999 (if calling from abroad, please telephone +441962 844 999) and they’ll put you in touch with a dentist who can help. Please refer to your Denplan policy document for full terms and conditions. Alternatively, you can try the NHS Urgent Care Service by dialling 111. First Aid Tips for Teeth Toothache What to do if you have bleeding following an extraction The first thing to remember is that it is normal to have some bleeding for the first day or so following an extraction. Many people are concerned about the amount of bleeding, however this is usually due to the fact that a small amount of blood is mixed with a larger amount of saliva, which looks more dramatic than it is. If you do notice bleeding, spit the blood out rather than rinsing your mouth. You will need to apply pressure to the socket – roll up a clean cotton handkerchief (do not use paper tissues), place it directly over the extraction site and bite firmly down on it for 30 minutes, whilst sitting upright. You can replace the pad if necessary. If the bleeding has not decreased after two hours, please contact your dentist or hospital for further advice. Following any extraction, it is important not to do anything strenuous and to avoid smoking and alcohol for the rest of the day. You may also find it useful to use extra pillows at night so that you sleep in a more elevated position. What to do if you lose a tooth in an accident If a healthy tooth is knocked out, there’s a chance it may be saved if you act quickly. Handle the tooth by the crown, not by the root, to avoid additional trauma to the tooth. If there’s debris on the tooth, gently rinse with cold water. Do not brush or scrub the tooth or handle it unnecessarily. Do not try to sterilize the tooth with soap, alcohol or mouthwash. If possible, try to reinsert (re-implant) the tooth into the tooth socket. Stabilize the tooth by biting down gently on a towel or handkerchief and get to a dentist or hospital as soon as possible. IMPORTANT – if a baby tooth (milk tooth) is knocked out, it MUST NOT be pushed back in. If you are unable to re-implant the tooth into the tooth socket then do not let the tooth dry out – if possible, keep the tooth in your mouth (between the cheek and gum) or put it in a cup of milk and get to a dentist or hospital as soon as possible. You can take painkillers but do not put aspirin or clove oil on the wound. What to do if you lose a Crown or Bridge If your permanent crown or bridge comes off, do not lose it or throw it away as we may be able to recement it for you. Keep the crown or bridge in something safe and contact us for an appointment. Your dentist will evaluate why it came out and also if there is any additional tooth damage or decay in your tooth before replacing it. Losing a crown or bridge can be quite inconvenient, especially if it affects one of your front teeth. The exposed tooth (or teeth) may also be very sensitive. As a temporary solution, and only if you feel it is safe to do so, you may find it useful to recement the crown or bridge yourself, until such time you can get to a dentist. Many pharmacists sell temporary crown cement, or you may also try a little bit of ordinary toothpaste or denture fixative. Seat the crown or bridge on your tooth (or teeth) as a test before cementing – using very light pressure, close your teeth together to make sure the crown/bridge is seated properly. The crown/bridge should not interfere with your bite in any way. If your bite feels very different or the crown/bridge does not have a secure fit, do not recement it. Never attempt to recement crowns or bridges with superglue. Your gums and soft tissues may react to the glue causing you pain, ulceration and swelling. The use of superglue can also make recementing the crown or bridge much more difficult, if not impossible, and you may then need a new one as a result. Broken Dentures Never attempt to mend broken dentures with superglue. Your gums and soft tissues may react to the glue causing you pain, ulceration and swelling. The use of superglue will also make repairing the denture correctly much more difficult, if not impossible, and you may then need a new denture as a result. If your denture breaks, please contact us so we can arrange to have it repaired correctly.
In order to join Denplan Care you will need to be classed as ‘dentally fit’. The dentist will assess your dental health and agree a programme of dental treatment with you (where necessary). Once the agreed treatment has been completed, you will be classed as ‘dentally fit’ and have up to 30 days from your completion date in which to join Denplan.
Most dental problems do not become painful until they reach a very advanced stage. Visiting the dentist on a regular basis will enable us to identify areas of potential risk at a much earlier stage. Early detection of an infection, plaque or decay can save you having extensive treatment later on, as we can help to prevent the situation getting worse. Early treatment generally costs a lot less as well.
Our dentists aren’t just checking the health of your teeth. At every examination we also carry out oral cancer screening, looking over the inside of your mouth to check for red or white patches or mouth sores. We also feel the tissues in your mouth and jaw to check for lumps or other abnormalities.
Dental X-rays x 2 = 1 day
Chest X-ray = 1 week
Barium Meal = 1 year
Nevertheless, X-rays will only be taken when clinically necessary, with your consent and following an explanation.
Gingivitis means ‘inflammation of the gums’ and is the earliest stage of gum disease. Plaque and calculus deposits on your teeth can irritate the gums causing them to become inflamed. They will appear red, swollen and shiny, and they may bleed when brushed. Gingivitis is completely reversible – if the plaque and calculus deposits are removed, your gums will recover. However, if left untreated, gingivitis may develop into periodontitis.
Periodontitis means ‘inflammation around the tooth’. The inflamed gums begin to pull away from your teeth leaving small pockets. These pockets trap food and plaque which is very difficult to remove with tooth brushing. The plaque and calculus build-up can cause further irritation, so the gum pockets get deeper and even more difficult to clean. Without professional cleaning the fibres and bone supporting the teeth is eventually destroyed by the bacteria in the gum pockets, you may also experience gum abscesses and pus may ooze from around the teeth. It is the loss of the supporting tissues that cause the teeth to loosen and eventually fall out or need to be extracted.
Unfortunately, unlike gingivitis, periodontitis is irreversible, although if detected early enough, professional dental treatment, advice and support can usually help prevent further damage and keep the conditional stable.
In the latter stages of gum disease you may notice that you have a bad taste in your mouth. There may be pus between the teeth and gums when pressed. You may notice a change in the way your teeth bite together and your teeth may be loose and painful, making it difficult to eat.
The best way to clean between the teeth is by using dental floss or tape, wooden sticks or interdental brushes, like TePe’s. Your dentist or hygienist can recommend a method that is most suitable for you. If you haven’t cleaned interdentally for a while, you may notice some bleeding to begin with. Don’t be tempted to stop cleaning as bleeding gums are usually a sign of inflammation (i.e. gum disease) – healthy gums will not usually bleed when you clean properly. Normally bleeding should subside within a week or two, as removing the plaque removes the cause of gum disease. However, if bleeding persists, contact your dentist as it may be caused by a build-up of calculus (tartar) which can only be removed by professional cleaning.
When we eat food or drinks containing sugar, the bacteria in our mouth turn it into acid. This acid attacks the tooth by dissolving and softening the tooth surface (enamel). The acid attack can last up to an hour after eating or drinking sugar, before the natural salts in your saliva is able to neutralise the acid, and allow the tooth surface to remineralise and harden. However, if you continuously eat foods or drinks containing sugar, your teeth become exposed to this acid for a much longer period, preventing the ability of the saliva to repair the damage. Over a period of time, repeated damage will become “tooth decay”.
In the early stages of the infection you may not feel any pain, however the symptoms of an abscess can range from a dull ache to severe pain and the tooth may be tender when you bite. Sometimes the infection can progress to the point where swelling threatens to block the airway, causing difficulty breathing. Abscesses can also make you generally ill, with nausea, vomiting, fever, chills and diarrhoea.
In order to save the tooth, and eliminate the infection, you would need root canal treatment. If root canal treatment is not carried out, the infection will spread and the tooth may need to be extracted.
The aim of the treatment is to remove the infected tissue from the root canal. The canals are thoroughly cleaned, shaped and disinfected and then sealed to prevent any further infection. Once they have been sealed, a permanent filling and/or a crown can be placed. Root filled teeth are ‘dead’ teeth which can be more brittle and prone to damage than ‘live’ teeth, so it is sometimes necessary to place a crown on the root filled tooth to support and protect it.
Many patients go to the dentist for an emergency appointment, get a course of antibiotics and start to feel much better. Then, because they feel well, they don’t return for further treatment. However, without treatment, the infected tissue remains inside the tooth causing the infection to spread again and the problem returns. Delaying treatment also reduces the prospects of success and it may prove impossible for your dentist to save the tooth at a later stage. Furthermore, repeated doses of antibiotics may result in them becoming less effective as you may gradually build up resistance to them.
Teeth are covered by a layer of enamel that protects the softer dentine underneath. If the dentine is exposed, the tooth can become sensitive. This usually happens where the tooth and the gum meet and the enamel layer is much thinner. Common causes of sensitivity are: –
There are many brands of desensitising toothpaste available to help ease the pain of sensitive teeth. You should use it twice a day instead of your regular toothpaste. You can also rub the toothpaste directly onto the sensitive areas with your finger.
Not everyone finds desensitising toothpastes helpful. Instead, you may want to try a non-alcohol mouthwash with a high fluoride content, like Fluorigard or Pronamel. They should be used twice a day after brushing – one of those times should be just before you go to bed, so the mouthwash doesn’t get rinsed away when you drink or eat something.
If you’ve been treating your sensitive teeth for a few weeks and have had no improvement, always contact your dentist for further help and advice. Your dentist will be able to investigate what is causing the sensitivity and find the best way of treating and preventing it. There are special desensitising products that your dentist may use to help relieve the symptoms. These can be painted onto the teeth to build up some protection. If this still does not help, your dentist may seal or fill around the neck of the tooth, where the tooth and gum meet, to cover the exposed dentine.
Crowns can be an ideal restoration for teeth that have been cracked, broken, or have been weakened by decay. A crown could be used for the following reasons: –
There are three main ways to replace missing teeth; partial dentures, bridges and implants.
There are three main ways to replace missing teeth; partial dentures, bridges and implants.
A partial denture is a removable plate with a number of artificial teeth on it. It may be all plastic or a mixture of metal and plastic. Dentures are held in place by their natural suction to your gums. They may also have clasps to help keep them in place in the mouth. Dentures are custom made to fit your mouth so you shouldn’t normally need a denture fixative, however, over time, dentures may become loose and not fit as well. When this happens, some people prefer to use a fixative for a short time before having them relined or replaced.
A dental bridge is an artificial tooth (called a pontic) that’s supported by the teeth at one, or both, sides of the space left by a missing tooth. A bridge is made in a dental laboratory and then permanently cemented into place with special adhesives. Unlike traditional removable dentures, a bridge cannot be removed for cleaning.
There are three main types of bridge; Fixed, Cantilever and Maryland.
A fixed bridge is the most commonly used. It is made by putting crowns on the teeth at either side of the space (abutments), and then joining these two crowns together by placing an artificial tooth (or teeth) in the space. This arrangement provides maximum support since any force applied to the artificial tooth when biting and chewing, is spread to the two supporting teeth.
A Cantilever bridge is similar to a fixed bridge but it is used where there is only supporting teeth available on one side of the space. It consists of two abutment crowns that are positioned side by side on the same side of the space. The artificial tooth is then connected to the two crowns, extending into the space. However, because a Cantilever bridge is only supported on one side, it limits its use to areas of the mouth which receive little stress during chewing.
A Maryland bridge (also known as a bonded bridge) is an artificial tooth that has metal flanges or ‘wings’. The wings are bonded onto the back of the supporting teeth either side of the space. A Maryland bridge requires minimal preparation to the supporting teeth, however it is not as strong as a fixed bridge so is normally only used for front teeth.
A dental implant is a titanium metal rod which is placed into the jawbone as a replacement for a missing tooth. It is used to support one or more artificial teeth in the same way that roots support natural teeth and, with the right care, they have been proven to remain in place for many years.
Having dental implants will involve at least one minor operation. Whether you can have implants will depend on your gum health and the condition of the bone in your jaw. Some dentists won’t offer you dental implants if you smoke as it can affect the outcome of the treatment. Implants are also less likely to be successful if you have a medical condition such as diabetes or osteoporosis, or have had chemotherapy, however a number of specialist tests to determine your bone health is required before proceeding with any implant treatment.
Causes – There are two main types of tooth discolouration; stains that appear on the surface of the tooth (extrinsic), and staining that appears within the structure of the tooth (intrinsic).
Professional tooth whitening products can help to lighten your teeth. They usually contain chemicals called hydrogen peroxide or carbamide peroxide. The whitening effects can last from a few months up to several years, however this varies from person to person.
Tooth whitening won’t work on false teeth, crowns, veneers or fillings (including tooth-coloured fillings). However, once your whitening treatment is complete, your dentist may be able to replace these with ones that match your new shade.
If you have tooth decay or gum disease, this will need to be treated before you have any whitening treatments. There are some other instances when your dentist may recommend that you don’t have your teeth whitened – for example, bleaching isn’t usually recommended for pregnant or breastfeeding women, or for anyone under the age of 18 whose teeth are still developing.
A veneer is a thin layer of tooth-coloured material which is custom-made to cover the front surface of the tooth. Veneers serve a mostly cosmetic purpose and maybe used to improve the colour, shape and position of your teeth, to help make them look natural and healthy. Because veneers are very thin and are bonded in place, very little preparation of the tooth is needed. Some types of veneers don’t need any preparation at all.
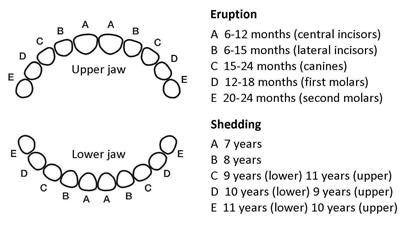
At the same time the two lower primary central incisors begin to loosen and fall out and are replaced by the lower permanent central incisors. Over the next six years (age 6-12) the remaining 18 primary teeth fall out and are replaced by permanent teeth. At about age 12 the four 2nd permanent molars appear behind the 1st permanent molars. The last teeth to appear are the 3rd molars or wisdom teeth. Not everybody has 3rd molars and there is considerable variation in the age at which they erupt but usually it’s about 18-25 years old.
Fissure sealants are a safe and painless way of protecting the biting surface of your child’s teeth from tooth decay, and they are capable of lasting many years. The process is totally painless and the teeth do not feel any different afterwards. Sealants are only applied to the back teeth, as these are the ones that have the pits and grooves which need to be protected. The process itself is quick and straightforward, taking only a few minutes per tooth. The tooth is thoroughly cleaned, prepared with a special solution and dried. The liquid sealant is then applied and allowed to set hard by shining a very bright light onto it.
Once sealed, your child’s teeth are substantially better protected from decay; however, it is essential that fissure sealants form part of an overall programme of dental care which includes daily brushing and attention to good dietary habits.
If you would like further information about fissure sealants, and whether the treatment would be beneficial for your child, please talk to your dentist who will be happy to advise.
As well as regular visits to the dentist, regular self-examinations are a simple, potentially life-saving process. Spend a few moments in front of the mirror looking in your mouth. Check your tongue, gums, lining of your cheeks, lips, under your tongue and the roof of your mouth. The most common warning signs of oral cancer are: –
Toothaches should not be ignored – if there is an infection, it can become severe if left untreated so always contact your dentist as soon as possible. Use dental floss to dislodge any food or debris that may be impacted. Clean the area thoroughly by rinsing your mouth with lukewarm (body temperature) salt water – do not use very hot or very cold water as this may inflame the gums. Avoid lying flat as this can raise the blood pressure and increases pain. If your face is swollen, apply a cold compress – you can make a cold compress by wrapping a tea towel around an ice pack.
Pain Relief for Toothache
The best over-the-counter painkillers for toothache are non-steroidal anti-inflammatory drugs, or NSAIDs for short. These include Ibuprofen, Diclofenac and Naproxen. DO NOT take Ibuprofen if you have asthma. Paracetamol or Aspirin are also good for dental pain, however, dental pain often comes from inflammation and pressure on various nerves and tissues, so, for this reason, NSAIDs can be better for dental pain because they are both pain relievers and good anti-inflammatories. Do not place Aspirin on the sore tooth or surrounding gums as it can burn your mouth and harm your teeth. Always seek help from a dentist as soon as possible.
Before taking any pain medications, always read the label for contraindications, side-effects and maximum doses, to make sure it is suitable for you to take. If you are unsure, always consult your dentist, doctor or pharmacist first.
 Priory Dental Care
Priory Dental Care